As we approach the end of the first quarter of a new Government, I’m taking a moment to reflect on a few papers and articles released and considering these against my experience of trying to use and implement Digital in the NHS.
I’m sure many of you will have seen or commented on the recent paper ‘Preparing the NHS for the AI Era: A Digital Health Record for Every Citizen’, as part of the Future of Britain policy initiatives. As usual, it was met with the full range of commentary, from enthusiasm and welcome support to the obligatory dumbing down headline about ‘chatbots doctors’. Dr Charlotte Refsum, Director of Health Policy, Tony Blair Institute for Global Change summarises the key points in her LinkedIn post (which is where most of my blog readers get their information these days since the demise of X – but that’s another story!)
Please can we fix the basic requirements first?
I totally understand the response: ‘Please can we fix the basic requirements first’. One of the biggest surprises when I joined the NHS 20+ years ago, was that the basic user requirements for tech were at least 5-10 years behind the nuclear industry that I had worked in previously. I recall being astounded at having to submit a business case for a £250 desktop multi-function printer/scanner to save hours standing at a photocopier, printing patient records, then re-typing that information into templates to be sent by email, and then yes, posting the paper records to the PCT HQ. My request didn’t get approved – I moved on.
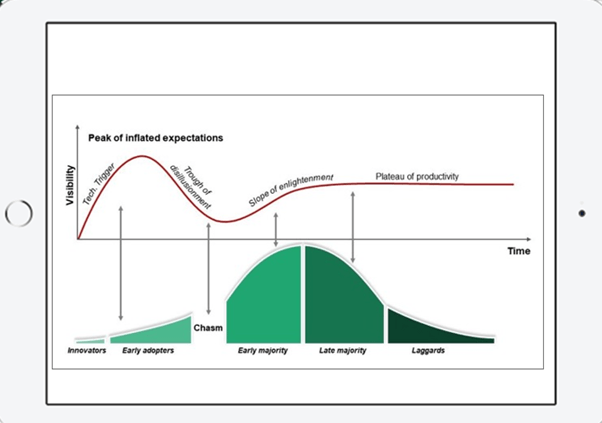
During those 20 years, we have seen variable improvements, some big-scale projects start, get delayed and then scrapped, and a lot of money paid for products not used. I use this image regularly in my presentations and it feels like the gap between the early adopters and laggards seems to be widening, as well as the hype increasing, quickly followed by the trough of disillusionment. I still take part in video meetings with practice teams, all huddled around one PC. No spider phone, or owl camera in the meeting rooms, and some don’t even have a webcam and headset to participate fully.
The Citizens Digital Health Record (DHR) and Primary/Secondary Care interface
I’ve been an advocate of patients having access to their full medical records for 10+ years since I worked in practice and could see the value to patients as well as to our workload. However, creating a new multi-sector DHR in light of the legitimate concerns around procurement and data security is not without challenges. Seeing the attempts to share and view patient data across health systems has been soul-destroying in some instances. The requirements of PCARP – ‘cutting bureaucracy’ and addressing the challenges of the primary/secondary care interface seem to be thorny too, with the bureaucratic referral process incorporated in the BMA collective action guidance. As a Commissioner in Cumbria in 2008 looking at part of this work, I recall a discussion with an Orthopaedic consultant defining the pre-surgery baseline test information they required. I asked why Primary Care couldn’t just create and supply a ‘view’ from the relevant part of the GP clinical system to Secondary Care. It has been technically possible for some time, but still not done. I still see each ICB or Region reinventing this wheel or worse, not addressing this issue at all.
The Technology Innovation Framework ‘new market entrant’ clinical system suppliers are still building functionality to send and receive ‘documents’ into and out of hospitals because they have to design the new systems to ‘fit’ with existing NHS systems and workflow. Secretaries spend hours listening to digital audio recordings and populating templates, administrators uploading or archiving the same, all to ensure the correct coded data is sent from A to B, or to make sure payments can be attributed for the work. This is light years behind where it needs to be in thinking and design. Why are they not designing these new systems to allow secure structured data flow and visibility, separated from ‘task handovers’, with a ‘patient friendly’ version alongside? I’m sure many of us have looked at our records in the NHS App and wondered what on earth some bits of it mean. So now, I’d say that people need access to their ‘health information’, not their ‘medical records’ – its subtly different. Clinicians need medical information in order to advise or treat, Managers need a different set again. Transferring care, is different from the information that patients need, as is the need to track flow of activity for demand, capacity and resourcing, and then capturing outcome data to check that the intervention works. It surely cant all sit in one DHR, can it?
Lord Darzi’s review
There will be many that comment on yesterday’s release of the Independent investigation of the National Health Service in England, AKA the Darzi review, for many it contains no surprises. This review along with numerous papers and articles all feature Tech or ‘Digital, not Analogue’, and AI as a central part of the solution. Those of us involved with change, implementation, and optimisation know, that the Tech alone will not suffice. Having the headspace to think differently, when you’re up against the clock, or burning out so you can’t even consider taking the risk of doing something new, all needs to be factored in alongside the Tech. Let alone addressing the working across silos.
Exhilarating and terrifying – not just the internet, but AI
Then I came across this old clip of David Bowie predicting the impact of the internet in 1999 and I have to say, I can have similar feelings about AI – it’s both ‘exhilarating and terrifying’ at the same time. I can get enthusiastic when I have a call like the one I’ve just had about predictive analytics, taking millions of data points and using AI to understand the trends. At the other end of this, I do more than roll my eyes when I see glib predictions that AI will solve all our problems, or replace the need for people, or be the only source of the truth.
Having worked with patient and staff data, and understanding the requirements of data controllership, the risk of data breaches seems a priority, closely aligned with clinical safety and acknowledging bias in all its forms. All the marketing hype is about efficiency, so it is great to see sensible guidance being released.
Dr Dave Triska offers his expertise with A Gold Standard Checklist for Healthcare Professionals Using AI & LLMs quickly turned into a super easy video by Dr Hussain Gandhi at eGPLearning. Both helping to highlight key tasks and risks for GP Partners & Practices, as they explore using these new technologies, whilst asking if the products popping up on the market are safe and secure.
Thinking Critically about AI in Healthcare from Dr Jess Morley is well worth a look at too.
As the system strives to move more and more services to digital platforms, leaving people behind, who may already be digitally excluded and suffer poorer health outcomes as a consequence, is equally important. Nexer Digital offers practical service design advice in this blog post by Chris Bush; AI for all; Inclusive design principles for the use on AI in the Public Sector and Danny Lancaster offers us real-world use cases to help us consider how AI tools can support a more inclusive workplace, not just a more efficient one.
So, with all of this in mind, we’ve decided to get the experts in the room and see how we can solve some of the core General Practice problems, using AI safely, inclusively, and effectively. When we asked people to tell us what problems they like addressed, it’s the mundane, repetitive, time-consuming things, not the boundary-pushing stuff.

If you’d like to join us at our Custom GPT Hackathon on 3rd Oct in Leeds, to learn, share knowledge, and maybe enjoy a pizza even whilst having fun, why not come along and find out which side of the David Bowie ‘AI line in the sand’ you’re on?

Meanwhile, I’m leaving you with an image of Dr Keith Grimes, staying up all night testing the new ChatGPT models in preparation.