As some of you may know, I try to improve patient experience and our NHS working lives through use of digital solutions. I’ve recently been on the receiving end of NHS treatment so thought I’d share the some of the missed opportunities for digital ways of working to help along the way.
The Problem
Sat morning; I found a breast lump, I wasn’t over worried as I’ve had them before, but knew this one would need checked out.
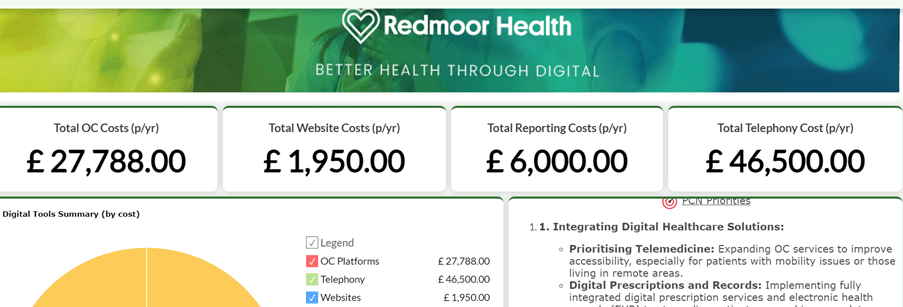
Appointment system – how much is online?
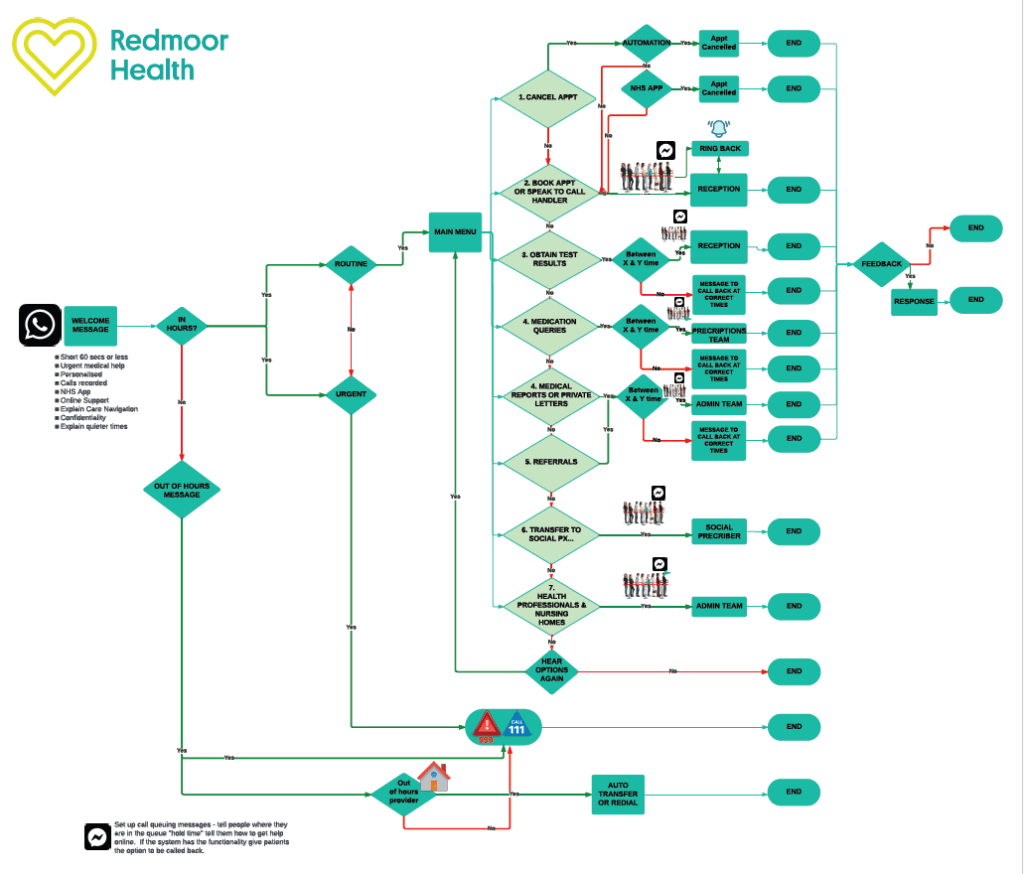
I logged onto the MyGp app to book an appointment with my GP and the next available face to face appointment was in 21 days. The next available telephone call: 15 days. Now, this is in a practice will full complement of GPs but with a fairly new manager who perhaps hasn’t yet got to grips with online services. I know this, because I’ve offered to go in and help. I’ve not received a call yet but I’m sure they have plenty of other stuff going on in the practice.
So I wait and ring on the Monday morning at 8.10am and ask for the soonest available appointment with a female GP – I’m happy to see anyone of 5 female GPs. ‘You can have one with a male GP in the extended access session this evening’. ‘No thank you, I really would prefer a female GP’ – I work with these people so not exactly keen to show male GP colleagues then sit opposite them in future meetings. I know they see bodies all the time, but still, I preferred to see a female GP. This happens all the time when you work in an area where you are also a patient. In our practice over 75% of our staff are patients, but as they have been in the same practice since they were children, they’ve sort of got used to it. Also, there isn’t anywhere else within 10mile radius.
Back to the call. The Receptionist tells me that there are no appointments available to prebook this week and asked if I had looked online. Of course I had, I did that first, I’m an advocate of working this way, I spend my working day telling everyone else to download apps and book online. So I advised her when the next available online appointments were and thought, perhaps they might want to look at that. I probably sounded grumpy – I apologise, but shouldn’t all reception staff be aware of when the next available online appointments are? How many reception staff actually know this information and if its fairly poor access, what can and do they do about this? Are they empowered to make more appointments available online or is the process for doing this fraught with lack of clinical system knowledge, unclear decision making, or just no appreciation of how helpful this is for patients and may save themselves some work? How do people like me, get over the threshold to show them these benefits?
I then explain to the receptionist (without being asked to) that I have a lump, that I think it will need seen and possibly referred and ask ‘what do I need to say or do to get an appointment this week, so that I am seen before Christmas please?’ ‘I’ll put you on the Emergency Drs list for a call this morning’. It’s not an emergency but if that’s the recommendation, I’ll go with that.
8.55am, the GP rings me back, I’m driving but I pull over and explain the problem. I’m asked how soon can I come in, I say ‘I’m passing in the next 5 mins or I am free later this afternoon, or on 2 more days this week’. The GP says ‘come in now’. Brilliant. Do all patients get this offer, or is it because its a fellow female colleague, or that they are Duty Dr that morning and has the surgery blocked out for these sort of problems? How many patients would know what to say to the Receptionist to get to this stage and how many would accept the first response of the wait?
The referral – is it really an e-referral system?
Skip a bit – on examination, ‘it’ needs a referral, GP says, ‘where would you like to be seen?’ I know this bit, so I reply ‘soonest one-stop-shop please’. ‘Oh, there doesn’t seem to be any sessions showing on the e-referral system so I cant book for you now, I’ll get the secretaries to fax it as a 2 week referral this morning and give you a call’ (yes, there it is for those of you who cant wait to Axe the Fax).
Do the hospitals not routinely show certain clinics on the e-referral system? What incentives and penalties are there in the contracts between CCGs and Acute trusts to help with this? We are being encouraged to use e-referral from General practice but what is happening in the hospitals? As for Axe the Fax toolkit- that’s possibly the subject of a future blog on its own.
‘Great’ I say, ‘if the secretaries give me the booking reference, I’ll do it on my app’ (MyGP app allows access to e-referral system now). ‘Erm, are you sure? I’ll get the secretaries to fax it and call you just in case’. This GP currently has interim Chief Clinical Information Officer responsibilities for our CCG. I get it that they are trying to make sure nothing gets missed, so appreciate this, along with their comfort with existing ways of working. At the same time why is there no confidence in this product or to try a different approach? Here was a missed opportunity to see how it worked in reality, then do something about it if it didn’t work smoothly. I’m always happy to be a guinea pig for the system, especially if it helps to improve or give confidence. Maybe it wasn’t the time or the place to suggest this on a busy Monday morning, so I didn’t offer and left expressing my appreciation for fitting me in so quickly.
Good old fashioned paper confirmation….
I didn’t receive any phone calls all week, but Thu morning, a letter arrived from Surgery (handwritten envelope, quaint but really? not even in an envelope with a window so you can see my name and address). How many practices still handwrite envelopes? I wonder what this costs in stationary, postage, staff time. They have my email address and consent to contact me by text. I resolve again to look at this in our practice to increase use of email/text/records access for confirmation purposes. I have access to my medical records so technically I would be able to see the referral information – of course only if the GP coded it correctly (I still haven’t got free text) and the letter was created and saved in a format that was viewable in the app. Another missed opportunity to test the system and gain confidence or feedback problems to the system.
The handwritten envelope contains my e-referral number and passwords for booking and confirmation of my appointment at 8.30am the following morning (Fri). Wow, now that’s quick, so I rearrange my stuff for the following day.
Now we are onto the Apps…
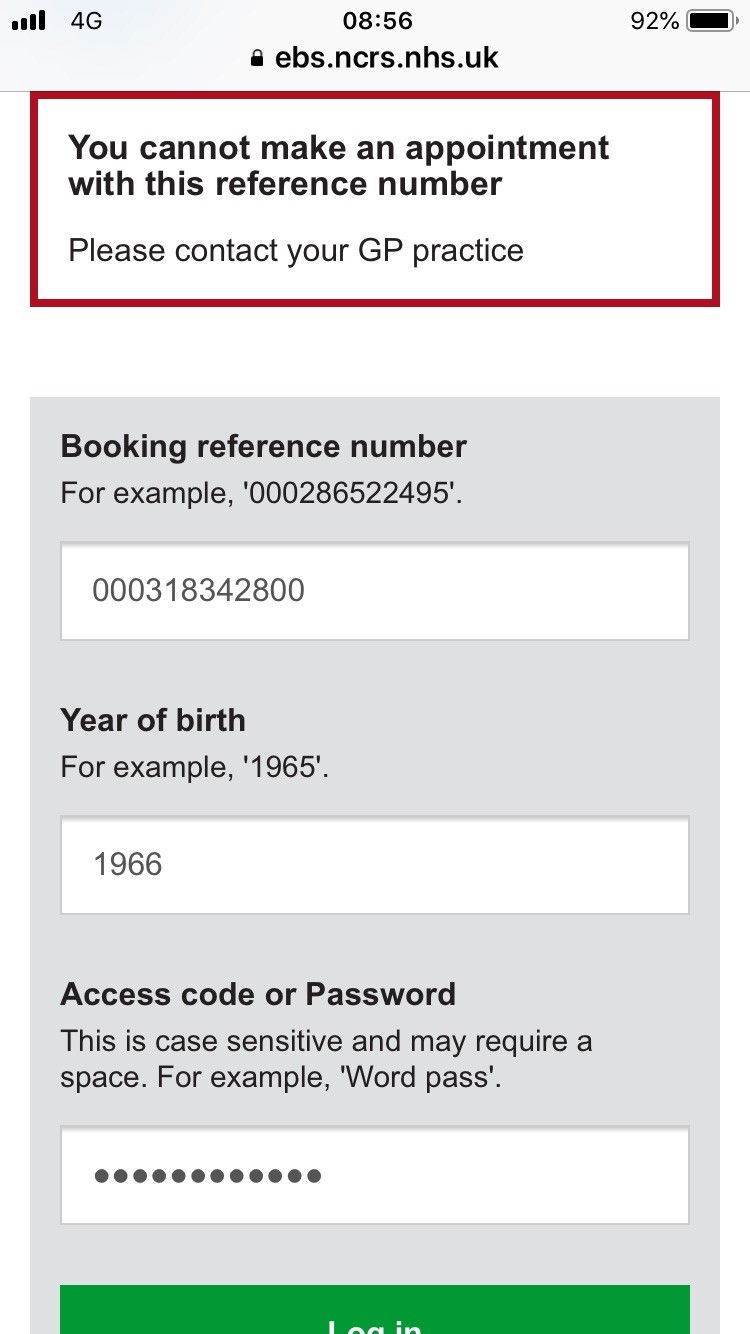
I have a play with the app anyway and this was the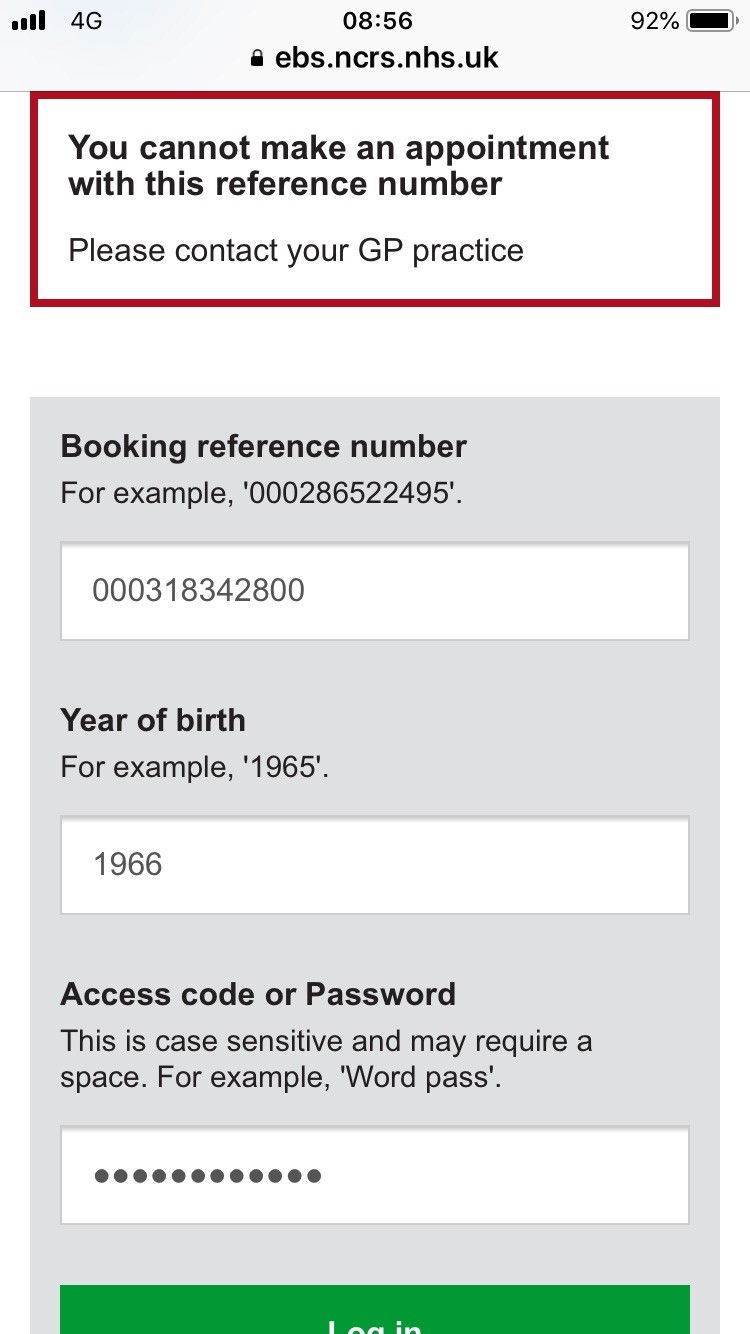 screen.
screen.
Is this an app problem or a practice configuration problem – how do I know who to ask? Will the NHS app solve all of this once the on boarding with my NHS credentials has been completed?
The appointment…(or not)
Fri morning, up early and after 1hr drive, I arrive at hospital at 8.20am. I go to the wrong check-in desk – its never clear is it from hospital signage, and get sent onto the next desk.
‘Sorry, it seems that your appointment is cancelled, let me check. It’s rebooked for 12th Dec’ (taking me into 3rd week since being seen). I ask when it was cancelled and I’m told on Monday 26th; the same day as it was booked. I might have been looking a bit unhappy at this point. I explain that I only received confirmation yesterday and ask who I need to call to rearrange – I’m given the Breast Clinic Secretary’s number. I can see the Breast Screening Clinic sign about 20m down the corridor and it does cross my mind to ask if I can go see someone there, but I don’t want to be pushy so I sit on the chairs a while then call the secretaries when they arrive at 9am. I explain, receive lots of apologies, and a promise to get a call later that day. This occurs around mid morning and I get another appointment in a week’s time.
The following day, Saturday, a letter arrives (from an outsourced mail system in Milton Keynes) advising me that my hospital appointment (for the previous day) is cancelled and to contact the booking centre to get a new date. I don’t bother as I’ve already got a new date, but intend to call the day before anyway to save another wasted journey. I do wonder though what system is in place to stop an appointment letter being sent after an appointment is cancelled? I know that booking confirmation texts can be sent immediately and that reminders are sent prior to the appointment, all giving the patients a chance to cancel or rearrange if things change. I realise that I hadn’t received a confirmation text in the first place.
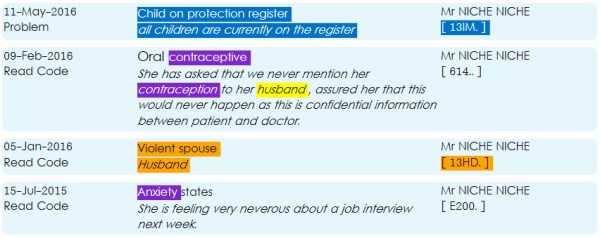
Mid week, I try to access my medical records so that I can see the dates that I have had this problem previously. There is a error with the system, so I email the system provider and I experience a bit of 3-way email/telephone ‘ping pong’ between EMIS, Patient Access and the Surgery. It appears that the Patient Facing Services isn’t working correctly and my record isn’t being updated in any of the apps that I use. The Surgery escalate this issue to EMIS but give me the medical details over the phone anyway after I explain why I need the information.
More letters and forms..
Another letter arrives to confirm my appointment (followed by a text message where I reply ATTEND to confirm that I will be there) and also containing a form to complete. This form asks for all the same information that I know has already been sent to the Breast clinic, in the standard 2 week wait referral template from the GP Clinical system. I know how much time Practices spend uploading these forms into the clinical system, archiving previous versions, ensuring that the forms auto populate with demographic and relevant medical information, then clinicians save it in the records for admin staff to send to the hospitals either in paper form or by fax, as well as storing in the e-referral system. Basically in triplicate. I duly fill in the paper form by hand, it asks if I have had any problems previously, what medication I take and for me to draw on the picture on the boobs where my lump is. The drawing actually looks like this.
 All of this information is already contained in the referral form sent by my GP.
All of this information is already contained in the referral form sent by my GP.
Roll on the clinic morning…
Arrived on time, checked in, sent to clinic, named ticked off on another list by a Health Care Assistant with a clipboard, ‘Have you got your form?’ she asks. I go to hand it over but she asks me to give it in at the next stage. I’m directed to another desk, where someone else checks me in by asking me for name, first line of address and asks me to take a seat. I wonder, why aren’t there any self check in screens in hospital. Also, if my confirmation letter had contained a unique bar code, this could have been scanned and avoided 2 separate check in steps thus creating time for people who prefer not to use self service or may need extra help. Even better if it was linked to the original referral – No?

Now for the showy off bit…
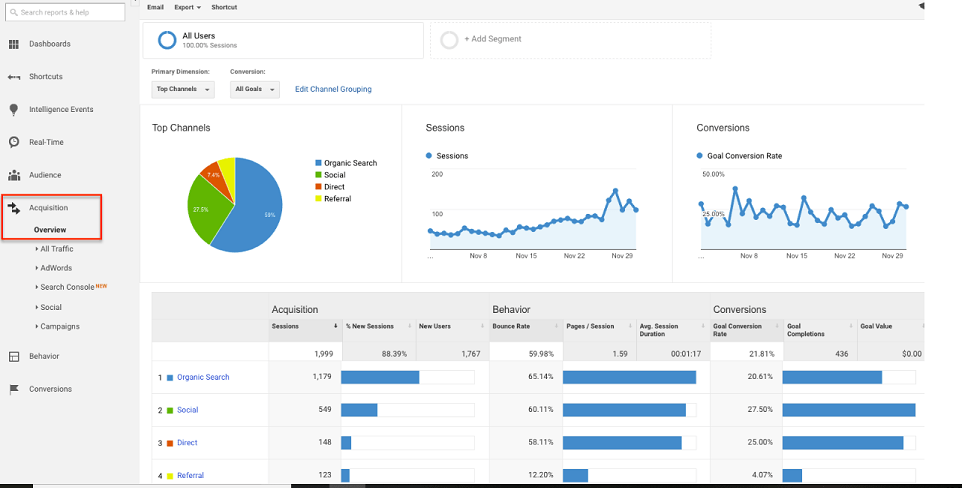
Here’s where I try to be an active citizen taking responsibility for my own health. So that I am prepared, I try to login to my medical records, of course I want to show people how this works in practice. NHS WiFi is apparently available in this hospital. I log in with my gmail address, but I cant access any of the apps to view my records. Is this is security policy and firewall protection? So I end up disabling NHS WiFi and switch to 4g. I can get through the app now, but these are my screenshots.


 Epic Failure!
Epic Failure!
I tweet a few of my mates to share my frustration.
I cant view any of the letters because they are scanned in a format that isn’t viewable. Disillusioned with online stuff, I give up and watch Homes under the Hammer on the TV screen. At least the rest of the walls are free from inappropriate posters. The previous week (the day before my cancelled appointment), I had attended the Radiotherapy dept with a relative and perhaps because I had this on my mind, everywhere I looked, there was a poster telling me how to ‘survive cancer’, or to join the ‘Living with cancer knitting & craft group’ etc. It made me want to remove any posters we have in our GP Surgery as its right ‘in your face’ if you are living with cancer or have a suspected cancer. Maybe hospitals and GP surgeries are not the place to bombard people generically with information booklets – what do you think?
My name is called and I’m collected by a Trainee Advanced Nurse Practitioner, who makes introductions and describes what will happen today. Before the examination, I’m checked who I am again, then asked if I take any medication and what for. I cant help myself at this point, ‘Don’t you get a letter from my GP with all of this information on?’ I cant see it anywhere in the cardboard folder that contains my hospital notes. I naively expect it to be on the top of the folder. A page of sticky labels is retrieved from the back of the folder and the clinician proceeds to stick one on each of the 3 separate pieces of paper. A yellow A5 one – for Ultrasound referral, a white one which is the same as the one that I had given in with the picture of the boobs on and another one for mammography. I wonder why two internal services attached to the Breast clinic need pieces of paper as further referrals? I also know these labels aren’t discarded when a patient changes GP as we often receive letters with the wrong GP information stuck on an old label. But someone had ‘ticked’ my GP name at the start so this person was confident to use the stickers.
The reply astounds me, ‘No, we don’t see that information and patients usually know what medication they are on, what if it was wrong in the GP system?’ Whoa – I’d hazard a guess that 80% or more of patients couldn’t accurately quote all of their generic medication names, quantity or dosage but possibly they could tell you how many a day, the colour or shape and maybe describe what they take medication for, i.e. my heart pills. And why on earth would they think that the GP records might be less reliable than the patient? This was a clinician in training, who is providing this training such that they are misinformed in such a way about the integrity of data held GP systems?
Best bit is still to come. On the screen, there is an online form with drop down boxes to select from and the clinician enters my verbal confirmation to the responses that are written on the form. None of the GP referral information seems to be available or visible in the hospital system – yet I know we have been sharing detailed care records in Cumbria between Primary, Community, Acute and Out of Hours systems since 2012. I know this because I have sat and painstakingly explained to patients why its a good idea to share and not to opt out because they may have unfounded worries about their health information being shared with pharmaceutical industries, for profit, without consent. Yet, why can’t this clinician see this information at the point of care and then confirm this with me, rather than ask again and go through the process of selecting drop down boxes? I can feel my blood pressure rising. The rubbish boob picture is there again on the screen and, wait for it, the clinician clicks on a ⊗ symbol and drags it on the screen to overlay where the problem is. I’m really struggling at this point to say nothing. Is this the limit of the IT skill in some parts of the NHS where someone has recreated a paper form into a flat undynamic electronic version using MS Word? I realise this is to create the electronic version of the paper form that I have drawn on and that no doubt mirrors the one that my GP drew on when creating the referral. But really, is that the way we create an electronic record?
When I’m examined, a marker pen is used to place a + on the lump – is this not an opportunity to photograph (clearly with consent) and insert the image? Could this have been done at the time of referral and included as an attachment by my GP? Not with a smiling head shot obviously, that would connect the breasts to the owner (making it a bit dodgy), but a real pair of boobs with X marks the spot, rather than these child like drawings, where it feels like we are all playing pin the tail on the donkey.
Now its time for the Robing Ceremony
Next, I’m taken to the Breast screening area, where I get a changing room, a basket for my stuff (like at the swimming baths) and a cotton gown to put on. I’m fairly rubbish at working out this sort of stuff. I’m not sure which way on it goes, the kind nurse tells me how to do it and apologises for the quality of the garment, explaining that they had lovely plush dressing gowns, but that didn’t make it back from laundry. It’s a good job I haven’t got large boobs as the gape was right in the chest area. After I had fiddled with the ties, she tells me that they fasten on the men’s side – I didn’t even know there was a gender side for fastenings but clearly that’s why I was confused after years of conditioning with ties on the left, not right.
The following procedures…
I could not fault the next steps. The whole team worked quickly and with empathy and care. The Radiographer was adept and very gently moved me to the right position for the mammogram and chatted to put me at ease. The Breast care nurse asked me what I did for a job, how far I had travelled, then apologised on behalf of the service for not hosting this nearer to home and also for the Receptionist at the first appointment who hadn’t thought it necessary to check if they could squeeze me in after the cancellation. The ultrasound confirmed the lump as a nice 2-3cm cyst. The Radiologist went ahead and aspirated, producing lovely green gunk (how on earth does that form inside your boob?), requiring no further investigation so I was discharged. I asked a few questions which were answered honestly and competently. Clearly, they are good at the clinical stuff.
After I was all finished, I found this on the wall in a different changing room and it made me chuckle.
 What a great idea, maybe make it into a video and play it on a screen instead of daytime TV.
What a great idea, maybe make it into a video and play it on a screen instead of daytime TV.








 screen.
screen. All of this information is already contained in the referral form sent by my GP.
All of this information is already contained in the referral form sent by my GP.


 Epic Failure!
Epic Failure! What a great idea, maybe make it into a video and play it on a screen instead of daytime TV.
What a great idea, maybe make it into a video and play it on a screen instead of daytime TV.  things to do, rather than just (as if its ever just) being a practice manager. I’d contacted the LMC a couple of years ago to see if there was any funded support for PMs, as there was a
things to do, rather than just (as if its ever just) being a practice manager. I’d contacted the LMC a couple of years ago to see if there was any funded support for PMs, as there was a  wondered aloud what criteria Sally uses to match people together. I had joked that I wouldn’t be an easy candidate, as I’m not sure I want to be a full time practice manager any longer and my reviewer had some trepidation too.
wondered aloud what criteria Sally uses to match people together. I had joked that I wouldn’t be an easy candidate, as I’m not sure I want to be a full time practice manager any longer and my reviewer had some trepidation too. s crying out for a
s crying out for a 



 but their earlier versions of their insurance reports were clunky so many practices were put off by this.
but their earlier versions of their insurance reports were clunky so many practices were put off by this.
