
I’m sure most of you will have seen the promotion, if not – here’s the Digital Primary Care Fest webpage again to see what you might have missed. Most of the content is being shared on the new Digital and Transformation network, so please join over 200 new users in the last two weeks, and chat along with like minded people who have questions and ideas to help each other.
Anyone who has organised a week of events will know the required planning and how much effort this takes. Not the wisest thing to do, but popping in 10 day holiday away and landing back in the UK a week before meant it was full steam ahead on my return. Although this added a certain amount of frisson, I’d recommend you avoid doing the same. Our team of keen and dedicated people, put in the effort to make the week a success, and judging by some of the comments on socials, I think everyone found something of use. And that’s what it’s all about, meeting people in similar roles, I think I saw the phrase ‘like-minded’ a lot, and the general energy throughout the days demonstrated that people had things to share and wanted to learn from each other.
I had the Custom GPT Hackathon to think about, but also attended the GP Federation/GP collaborative event, and the Empowering Digital & Transformation Leads day in person, also joined the launch of the D&T Network, and the session on the White Paper, digital transformation in primary care; sharing insights from 2 years usage across 1700+ practices. By the end of the week, I was both buzzing and very tired – I’ll blame that on delayed jet lag!
What did I learn?….
GP Provider Collaboratives (often built from Federations and Alliances of practices) in some areas still seem to be missing out of the ‘engagement’ loop in between ICBs and Practices/PCNs. In addition to being Providers in their own right, for Enhanced Access and other ‘at scale’ services, many also employ the Additional Roles and the workforce element is resource heavy for them. As ‘membership’ or representative organisations, they have a crucial role in engaging with their practices, which Commissioners could and should exploit. This seems particularly important when trying to deliver consistency of services and access, across neighbourhood teams or using common digital products within networks, to offer equity of access beyond core hours.
The ability to communicate at scale is also an opportunity. Federations and Collaboratives can do this and ensure consistent information is delivered about primary care services at ‘Place’ or neighbourhoods, supporting practices and PCNs, using content shared across Websites and Social Media. Listening to the conversation about GP websites, I was transported back to 2017 and watching 9 practices independently create their own version of information about a new same day service, then posting it separately on 9 different websites. I’m not suggesting a separate website is needed for Enhanced Access, but I am still suggesting that content is created by the service provider, then pushed out once, across a common website platform, directed to and from GP websites, which is where patients will look to find out about appointment availability. It’s still uncommon to see fully integrated evening and weekend appointment availability with the full primary care team, accessible to book online via a GP website. Whilst there are great examples around where some Feds have got a hold of this, most are still on the first page.
Data – who’s uses it and why?
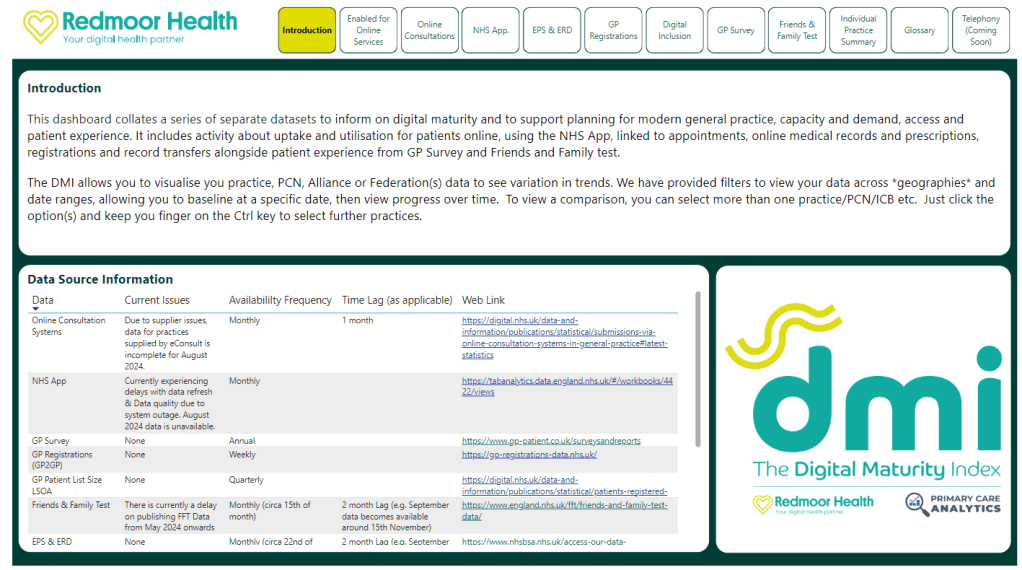
On both the GP Collaborative day and the DTL day, I shared our Digital Maturity Index, which we have just refreshed to include Online consultations and will incorporate telephony data in the new year. There was acknowledgement in the room about the variation across practices, with nods of recognition of practices who may be further behind on their digital journey. We always have an interesting discussion when I compare GP survey responses against Digital access. But looking at the Registration with a GP Surgery and spotting where Collaboratives can support working beyond just the practice, we could see opportunities to help with coding and summarising, also smoothing the Registration process across the practices. Someone suggested that the ICB would find this data useful, and yes, perhaps through the lens of contract monitoring, I’m sure they would. At the same time, the Collaboratives and PCNs will be impacted by the success or failure of their member practices. Relationships still seem to be a source of tension, as different primary care provider organisations work out their purpose and collective benefits.
The DTL (Digital & Transformation Lead) day.
We wanted this to be a day where DTLs shared their challenges, helped each other, offering suggestions about things that had worked well, and the DTLs were certainly active in this process. I don’t know why, but I was surprised how many DTLs were ex or still acting Practice Managers. I would have looked to move into that role myself if I’d not already joined Redmoor and we lost two great colleagues to the role when the jobs were first created. The DTL role is very much like practice management, hearing comments about feeling ‘quite isolated’, and needing to influence stakeholders at varying levels of seniority across organisations (ICBs, Clinical Directors, GP Partners, PCN managers, & practice teams). Not so easy to do though, when not necessarily directly managing. Others expressed a lack of clarity of expectation of the role both from commissioning and provider organisations, without much structure for development and very much relying on own resilience. Some great ideas came through to maximise income for practices and PCNs, while still ‘ticking the ICB contract boxes’, and delivering time-saving initiatives in practice, that improve the patient experience. I’m sure my colleague Dillon Sykes will have a blog coming out about his last two weeks, so I’ll leave him to share his thoughts too.

Now for the #Hackathon
The GPT Hackathon day was just the best for me, largely helped by the people in the room who needed little prompting to show their innovations. It was great to catch up with and see many familiar faces and to meet new people, whom I’ve only known online. As ever, the quality of the speakers and contributors kickstarted the thinking, with the morning devoted to learning all about AI and GPTs and the afternoon spent putting that learning into practice to come up with use cases. A big thank you to Dr Keith Grimes, Curistica, and Chris Bush and Lee Valentine, Nexer Digital. We had a range of Tech enthusiasts, patient representatives, and inclusion specialists with us, alongside people who wanted to explore how GPTs could support them in daytime workload. Some great ideas were sent in beforehand, in case the teams in the room ran dry of ideas, but a few wanted to use the opportunity to pitch ideas, before breaking out into groups to build. I was amazed at how quickly everyone put the morning’s learning to good use and all teams delivered a solution in just 1.5 hrs.

My colleagues Matt, Clare, Dillon, Stacey and Leoni were able assistants on the day and Matt recorded most of the sessions. You can find Matt’s more detailed blog from the day containing the slides and videos if you want to have a more detailed look.
The learning for me is that we have a void of ‘governance’ that is leading to caution in many and on the flip side, people possibly working outside the ‘safety zone’, not understanding the risks or personal liabilities. One of the hacks was to create an AI marketplace, where people could visit to find out more, where suppliers could offer support and clinical safety, alongside governance guidance. They built a quick GPT for suppliers to check if their product needed DCB0129 & DCB0160. I can see a need for a follow-up round table event with representatives from ICO, CQC, Regulators, Medical Defence unions, Medical, Nursing & Management representative organisations, alongside NHS as Commissioners and Standards organisations. Then we can explore where the concerns may be, what the actual risks and liabilities are vs those as perceived and who these currently sit with, and who they might be covered by in the future. Until we move this away from independent practitioners to the wider NHS system, we cant harness the opportunities that AI can bring or manage the safety at scale. I posted on the NHS AI forum afterward and the suggestion of building an ‘AI Charter’ together might help us all.
Always great to feel like you’ve delivered something that makes a difference, so sharing a few posts from others who enjoyed the day, Dr Amar Ahmed, Dr Sheikh Mateen Ellahi, Dr Andrew Noble, Dr Stuart Berry, Dr Chris Nortcliff and Chris Bush.
Finished with a pint to celebrate – sorry for spoiling the photo with my eyes closed but like to be consistent 🙂
Drop me a line if you want to put your name down for the next session.